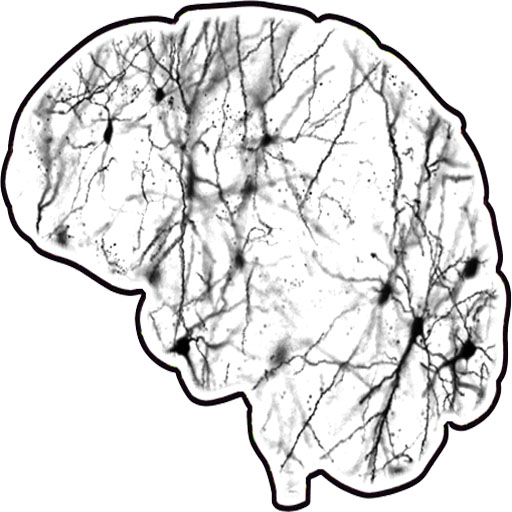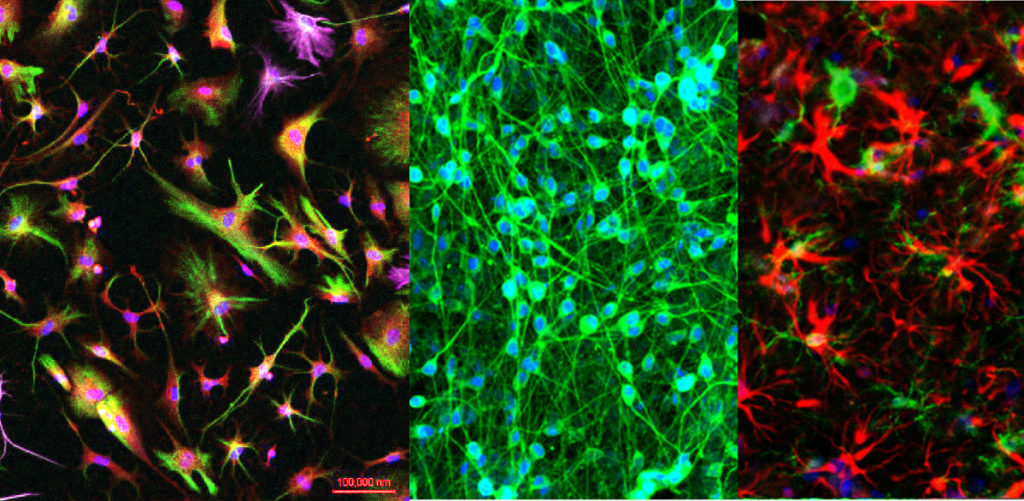
Alzheimer’s disease (AD) is a neurodegenerative disorder characterized by dysfunction and deterioration of neurons resulting in loss of memory and progressive cognitive decline. Current treatments are aimed only at symptom management. Three barriers to effective therapeutic development include: 1) a lack of definition of the heterogeneity of AD pathogenesis, 2) a lack of highly predictive biomarkers to facilitate early intervention, and 3) a need to identify pathways involved in cognitive decline and AD that can be targeted for therapeutic intervention. We are using induced pluripotent stem cell (iPSC) technology coupled to comprehensive studies of patient populations to interrogate the cellular and molecular mechanisms underlying AD in an effort to break down these barriers. We propose that there exist multiple forms of AD that have different underlying causes, and that multiple therapeutic interventions may be needed to address disparate etiologies. In collaboration with NYSCF and Rush University, we have generated 50 iPSC lines from two cohorts, the Religious Order Study (ROS) and the Memory and Aging Project (MAP). Under this project, we are studying these lines, with a focus upon three subsets of subjects that lie on the extreme ends of the pathological spectrum: 1) no brain pathology, not cognitively impaired, 2) high pathology not cognitively impaired, and 3) high pathology, late onset Alzheimer’s disease. In addition, we have generated and/or collected iPSC lines from familial Alzheimer’s disease subjects, which we analyze in parallel. We are measuring AD relevant outcomes (Aβ, p-tau, cytokines/chemokines) and acquire unbiased transcriptomic and proteomic data from in vitro differentiated neurons, astrocytes, and microglia from these individuals. These data will be integrated with clinical data, neuropathology data, and genetic data acquired from the same subjects from whom the cells were derived using multiple computational approaches. We hypothesize that: 1) A subset of pathological findings in the postmortem brain can be predicted by cellular phenotypes measured in vitro from neurons and glia derived from the same subject and 2) Network analyses of iPSC-derived neurons and glia at the transcriptomic and proteomic level will define subgroups of humans that predict neuropathology and cognitive status. Through these studies, we aim to evaluate whether iPSC-derived cells can act as a diagnostic or prognostic tool for cognitive decline and AD and begin to address the cell and molecular mechanisms underlying heterogeneity in late onset Alzheimer’s disease.